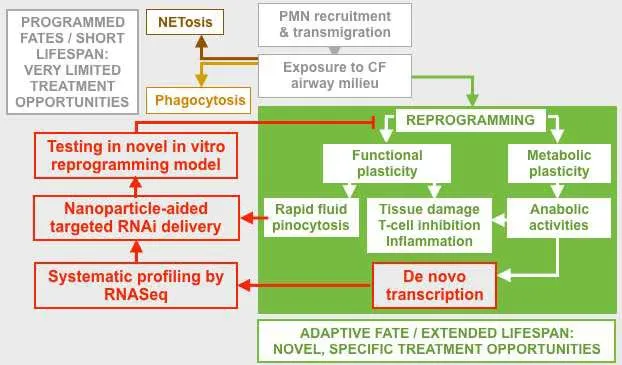
This project aims to identify therapeutic targets in pathogenic polymorphonuclear neutrophils (PMNs), an inflammatory subset that destroys airways…
PI
Rabindra Tirouvanziam & Greg Gibson
Publications
Margaroli, C., Tirouvanziam, R., “Neutrophil Plasticity Enables the Development of Pathological Microenvironments: Implications for Cystic Fibrosis Airway Disease”, Mol Cell Pediatr 3, 38 (2016). https://doi.org/10.1186/s40348-016-0066-2.
Research Area

